Now that we’ve covered the basics of health insurance in our eight prior installments of our Understanding Your Insurance Series, we thought it might be time to dig a little deeper.
What is a specialist, and why would I need to see one as opposed to my regular doctor?
 To understand what a specialist is, we should define what a “regular doctor” is first. The definition of a Primary Care Physician (PCP) or General Practitioner (GP) is: a medical doctor who is trained to provide primary health care to patients of either sex or any age. With that being the case, why would you ever need to see any other kind of physician, right? Well, there are certain conditions or health requirements that may best be seen by a specialist in that area.
To understand what a specialist is, we should define what a “regular doctor” is first. The definition of a Primary Care Physician (PCP) or General Practitioner (GP) is: a medical doctor who is trained to provide primary health care to patients of either sex or any age. With that being the case, why would you ever need to see any other kind of physician, right? Well, there are certain conditions or health requirements that may best be seen by a specialist in that area.
The definition of a physician specialist is: a physician who focuses on a specific area of medicine or a group of patients to diagnose, manage, prevent or treat certain types of symptoms and conditions. These physicians have usually received additional years of education within that specialty. Take allergy/immunology for example. To become a certified allergist, you must not only attend undergraduate and medical school, but you must also complete two more years of specialty training in allergy and immunology. Therefore, if you are struggling with severe allergies or immunology related illnesses (asthma, eczema, hives, etc), it’s usually best to be seen by an allergist. Another good example is an oncologist. If you find yourself having been diagnosed with cancer, you would most certainly want to be seen and monitored by an oncologist who is versed in your type of cancer and its treatment.
So can I just go and see whatever specialist I want?
In most situations you would be seen by your general practitioner for your symptom or condition first, unless you are forced to go to an urgent care or emergency room. In either case, your physician at the point of treatment, will determine if you need to receive further care from a specialist. In many cases, this means your PCP will need to refer you to a specialist. It is important to note, if your insurance plan requires a referral, and you don’t get one from your PCP first, your insurance won’t cover the cost of seeing a specialist. In most cases your PCP, and even most Urgent Care and Emergency Rooms, will have a list of specialists to whom they frequently refer and trust.
How do I know if my insurance requires a referral?
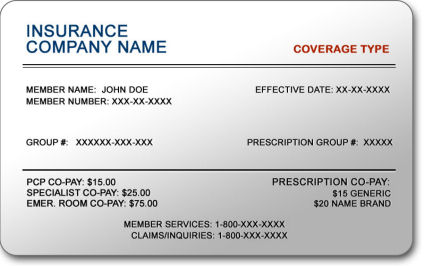 As we’ve mentioned so many times throughout this series, the best way to know if your insurance requires referrals is to contact your insurance carrier directly. The phone number should be located right on your insurance card. Your insurance card may even indicate if you require a referral directly on the card itself.
As we’ve mentioned so many times throughout this series, the best way to know if your insurance requires referrals is to contact your insurance carrier directly. The phone number should be located right on your insurance card. Your insurance card may even indicate if you require a referral directly on the card itself.
So what is the process for getting a referral?
 As mentioned above, you generally need to be seen by your PCP for the condition and he/she will then refer you to a specialist if necessary. Either your PCP, insurance company, or in some cases the specialist, will let you know when the referral is approved and you will usually receive an approval letter in the mail from your insurance company. Referrals are generally good for 90 days or up to one year. The most important thing to remember is that the referral is approved prior to being seen by the specialist or you run the risk of your insurance not covering the cost of the appointment.
As mentioned above, you generally need to be seen by your PCP for the condition and he/she will then refer you to a specialist if necessary. Either your PCP, insurance company, or in some cases the specialist, will let you know when the referral is approved and you will usually receive an approval letter in the mail from your insurance company. Referrals are generally good for 90 days or up to one year. The most important thing to remember is that the referral is approved prior to being seen by the specialist or you run the risk of your insurance not covering the cost of the appointment.
Hopefully this clears up any questions regarding specialists and referrals. Our next installment will cover considerations when changing insurance plans.
Category: Uncategorized


